The UN general assembly recognised drug-resistant infections in 2016 as one of the greatest threats facing humanity. And in May 2017, G20 leaders called for national action plans by the end of 2018 – plans set in train by the World Health Organisation in 2015. But momentum is already being lost. Commitments are the first step, but nothing will be achieved if they are not translated into action.
Analysis by Wellcome and the UN Foundation shows that 151 of 195 countries are developing a plan. However, only half address the threat across human and animal health and the environment, and only one in five commit to reducing antibiotic use, improving hygiene and preserving antibiotics of last resort. Most tellingly, only 5% are adequately funded and monitored by the governments responsible for them.
Yet still, too few new antibiotics are in development. CARB-X is a new partnership supporting 18 new potential treatments, but progress is still slow. If future generations are to benefit from antibiotics, more investment is required.
Meanwhile, the superbugs are progressing rapidly. Since the UN declaration, they have killed about 700,000 people worldwide. In Nevada in 2016, a 70-year-old woman died after breaking her leg, which later became infected with a superbug resistant to 26 antibiotics. In South Africa, multidrug-resistant TB is spreading. In the UK, untreatable strains of gonorrhoea are on the rise.
Politicians and scientists have an urgent role to play but they cannot solve the problem alone. Tackling drug-resistant infection is everyone’s business. The threat transcends that of HIV, TB and cancer.
In recent years, warnings of antibiotic resistance, improper and overuse of antibiotics and the dire need for new treatments have become familiar. But what has often been missing from this rhetoric is a focus on improving access to antibiotics to all who need them. This complex mixture of better prescribing twinned with better access is complicated and requires nations to act in a way which fits their needs.
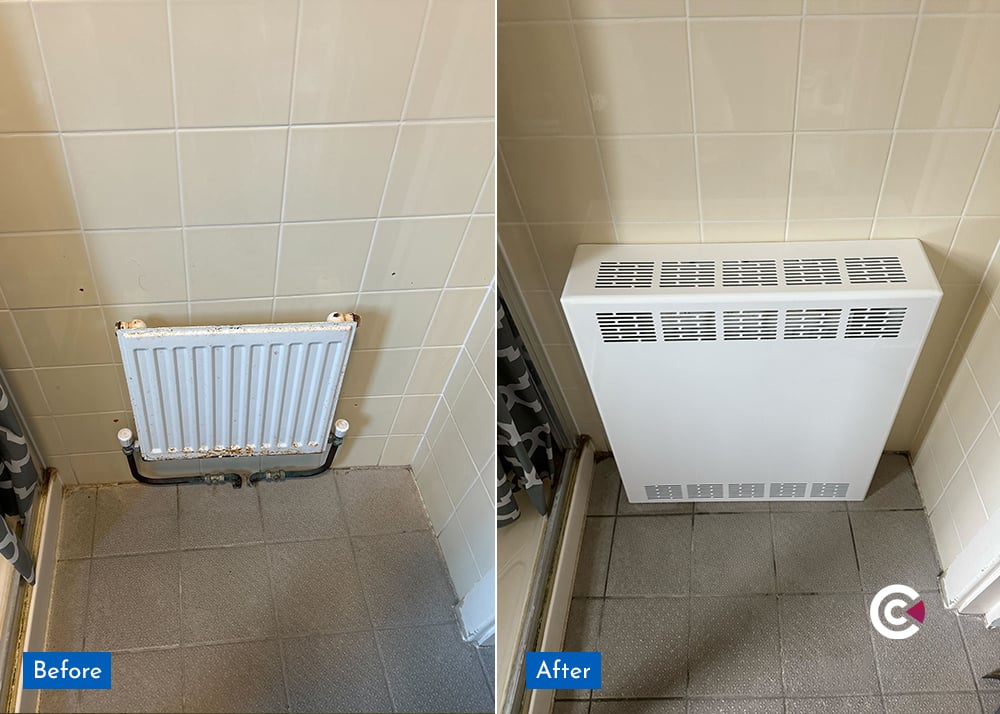
To stop superbugs undermining modern medicine, to prevent lives being lost through lack of access to effective medicines, action must be taken, and we must act now. Part of the solution is improved education and cleaner environments. Contour was the first adopter of anti-microbial technology in the low surface temperature market, using BioCote on it's very first LST Radiator Cover in 2003, and every single one supplied since which has provided cleaner and safer healthcare environments across the UK, helping in the fight against hospital-acquired infections.

This article was adapted from an article by Ed Whiting in The Guardian dated 8th October 2017. Ed Whiting is director of policy and chief of staff at the Wellcome Trust.
-1.png)
















/anti-ligature%20vent%20grilles.jpg)